
Schools and Departments
La Trobe's Schools and Departments are known for making a positive difference in the lives of our students, partners and communities.
Our distinctive course portfolio embraces diversity, flexibility, equity and accessibility – and provides students with the knowledge and skills they need to work effectively in local and international settings.
Find out about our Schools and Departments

The School of Agriculture, Biomedicine and Environment is cultivating healthy food, healthy people and healthy ecosystems in Australia through excellence and innovation in education and research.
Our goal is to advance research and teaching in the biological, biomedical, environmental, molecular and chemical sciences.
Our education programs are flexible, contemporary, interdisciplinary and industry-engaged and achieve the right balance of theoretical and practice-based teaching.
Our researchers work collaboratively with our partners in industry, clinical organisations, philanthropy and government to achieve research outcomes that have a positive impact on the communities we serve. We bring together the right capabilities, manage projects efficiently, act with integrity, and turn research results into translational outcomes.
Websites
School of Agriculture, Biomedicine and Environment Baker Department of Cardiovascular Research, Translation and Implementation Department of Biochemistry and Chemistry Department of Ecological, Plant and Animal Sciences

La Trobe is changing the face of health and wellbeing in Australia and abroad. Our teaching and research programs in the School of Allied Health, Human Services and Sport are helping to build quality health systems that, in turn, build healthy communities.
We foster lifelong learning for health professionals through undergraduate, postgraduate, and graduate research degrees and continuing professional development programs that equip them to upskill, reskill, advance into leadership roles or pursue research.
We also provide students with access to an extensive network of healthcare services and industry partners. Our outstanding placement programs provide future health professionals with real world experiences.
Our researchers specialise in most areas of allied health including sport and exercise medicine, social inclusion of people with cognitive disabilities, and the treatment of aphasia and stroke.
Websites
School of Allied Health, Human Services and Sport Department of Community and Clinical Health Department of Physiotherapy, Podiatry, Prosthetics and Orthotics Department of Sport, Exercise and Nutrition Sciences

The La Trobe Business School is enhancing learning through education and research that is future-focused, applied, innovative and responsible.
Our goal is to become one of Australia’s pre-eminent business schools as measured by our innovative courses, the success of our graduates, the positive social impact of our research and the strength of our partnerships.
Through our worldwide network of partnerships and collaborations, we are uniquely positioned to deliver innovative solutions, to act on opportunities, to educate the next generation of ethical business leaders and produce impactful research that benefits business and society.
We use the United Nations Sustainable Development Goals and the United Nations Principles for Responsible Management Education to guide everything we do.
The result: We graduate professionals with a commitment to positive social impact.
Websites
La Trobe Business School Department of Accounting, Data Analytics, Economics and Finance Department of Management and Marketing
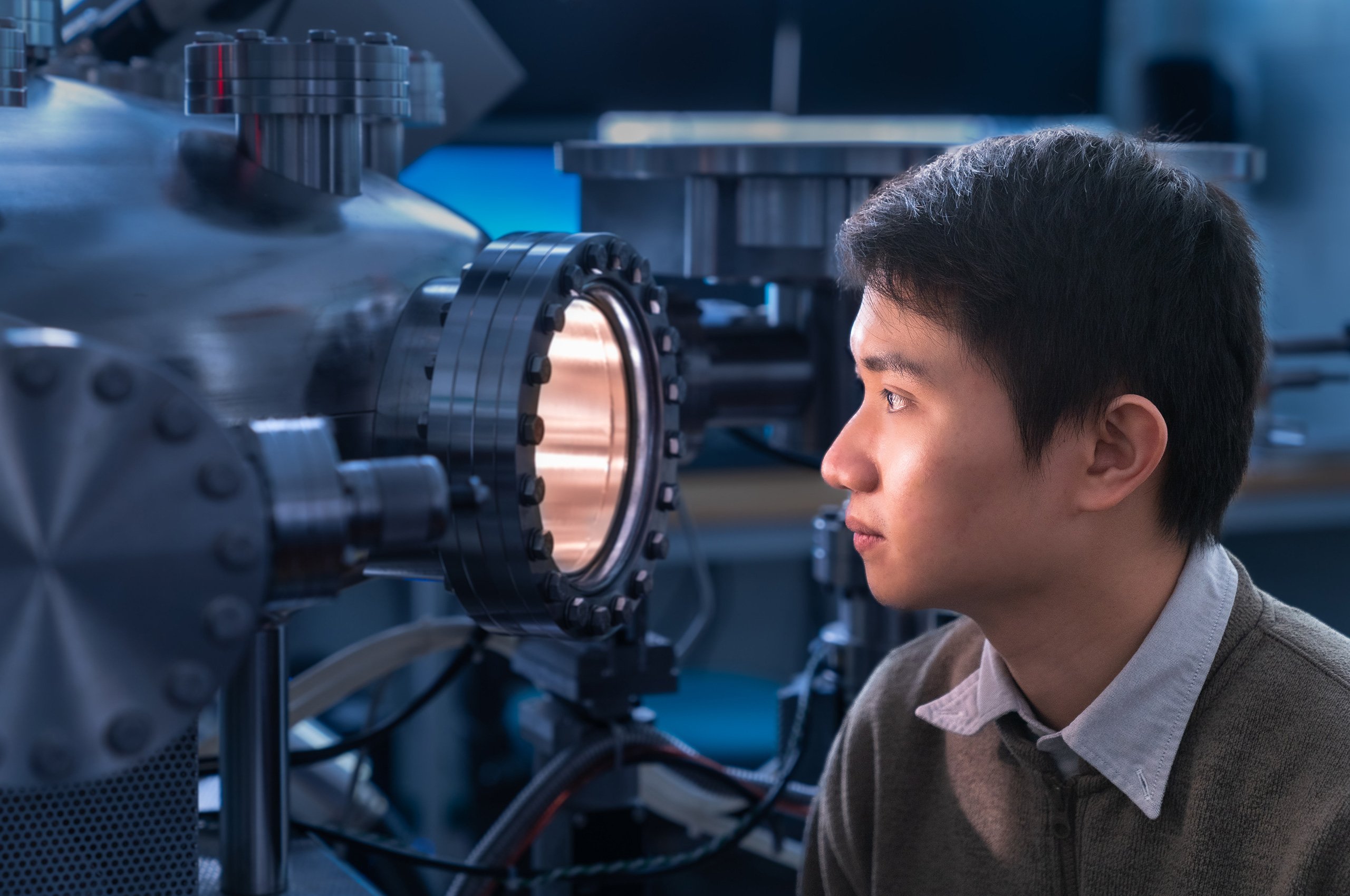
The School of Computing, Engineering and Mathematical Science offers high quality teaching and research programs to advance knowledge in engineering, computing and mathematical sciences.
Our programs train graduates to meet the need for an adaptive and technologically trained workforce. We do this by carefully designing our programs in consultation with industry. Our laboratories and facilities provide students with hands-on experience that complements their theoretical training.
Our key areas of strength include artificial intelligence, cybersecurity, data science and mathematical modelling, infrastructure and advanced manufacturing. We champion cross-disciplinary research in health, infrastructure and agriculture to positively impact our communities. We also have recognised research expertise in engineering, computing and mathematical sciences.
Websites
School of Computing, Engineering and Mathematical Sciences Department of Computer Science and Information Technology Department of Engineering Department of Mathematical and Physical Sciences

La Trobe is changing the face of education in Australia and abroad. As a leader in the industry, we are building a quality profession for all.
Our vision is to prepare high quality education professionals who want every learner to reach their full potential. Our success is directly linked to our outstanding partnerships with schools, early learning centres and other education providers.
We foster lifelong learning for education professionals through undergraduate, postgraduate, graduate research degrees and continuing professional development programs that give them the tools to upskill, reskill, advance into leadership roles or pursue research.
We are also recognised for leading contemporary education debates. Our role in promoting evidence-based approaches to quality teaching and impactful learning is recognised nationally and internationally.
Website

The School of Humanities and Social Sciences is a dynamic community of scholars who research and teach about the human experience – from its earliest beginnings to the latest developments in society, politics and culture.
We are known for our outstanding teaching programs that broaden students’ intellectual horizons, strengthen their career prospects and improve the societies they serve. Our coursework programs centre around the Bachelor of Arts, which offers students one of the widest ranges of majors in the country.
We offer students outstanding placement opportunities and exposure to industry projects so that they graduate with workplace experience, a commitment to professional responsibility and high ethical standards.
Our scholars are world leading researchers who study the human experience from its earliest beginnings to the modern day, here in Australia and around the world.
Websites
School of Humanities and Social Sciences Department of Archaeology and History Department of Languages and Cultures Department of Politics, Media and Philosophy

The La Trobe Law School’s progressive and practical courses ensure that graduates are career ready – and ready to make a difference in their local and global communities.
We offer undergraduate programs in Law and Criminology – including a range of double degrees – at La Trobe’s Bundoora and Bendigo campuses. We also offer postgraduate Law at our City campus, Masters by research and PhD programs.
We partner closely with community legal centres, law firms and criminal justice organisations. Our outstanding clinical placement program ensures that students graduate with valuable workplace experience, a commitment to professional responsibility and high ethical standards.
Our staff are research leaders who produce high impact outcomes. We have a strong commitment to the rule of law and community service, and use our findings to advise on and drive law reform in Australia and overseas.
Website

The School of Nursing and Midwifery has a long and proud history as one of the oldest tertiary nursing schools in Australia.
We offer education programs in nursing and midwifery that foster lifelong learning including undergraduate, postgraduate, research higher degrees and continuing professional development programs.
Our goal is to improve community health and wellbeing locally, nationally and internationally, by producing outstanding graduates, and research outcomes, that set best practice in the disciplines of nursing and midwifery.
We also recognise our role in promoting global health outcomes and maintaining a strong international footprint. Our students are encouraged to engage internationally through placements and mobility programs. Our staff offer professional training through partnerships that build clinical knowledge.
Website

The School of Psychology and Public Health offers quality teaching and research programs to advance knowledge in Psychology, Counselling, Therapy and Public Health.
We are known for our distinctive course portfolio that embraces diversity, flexibility, equity, and accessibility – and provides students with the knowledge and skills they need to work effectively in local and international settings.
We work closely with our extensive network of healthcare services and industry partners to offer practice-based education that builds knowledge and delivers outstanding graduate employment outcomes.
Our School also produces impactful research that is multidisciplinary, covers the entirety of the life course, and ranges from being person-centred to population based.
Websites
School of Psychology and Public Health Department of Psychology, Counselling and Therapy Department of Public Health

The La Trobe Rural Health School aims to Make Rural Health and Wellbeing Matter locally, nationally and internationally through graduates and research outcomes that make a difference.
We foster social justice through engaging with the health and wellbeing of rural communities across Victoria recognising strengths and needs. We define rural as any region outside of a major Australian metropolitan city and are proud to be based on each of La Trobe’s regional campuses in Albury-Wodonga, Bendigo, Mildura and Shepparton.
The School is distinctive for being entirely based in the regions, and graduating students from many health disciplines back into the rural Victorian health workforce.
The La Trobe Rural Health School aspires to be not only Australia’s largest rural health school, but also Australia’s best rural health school as measured by our graduates’ success as rural healthcare professionals, and our research rankings.
Website
