Hypertension and Immunobiology Research
Hypertension or high blood pressure is a serious medical condition that can increase the risk of heart attacks, strokes, heart failure and kidney disease.
Hypertension or high blood pressure is a serious medical condition that can increase the risk of heart attacks, strokes, heart failure and kidney disease. It affects approximately 40 per cent of the world’s adult population and is one of the major causes of premature death. Current approaches for treating hypertension include lifestyle modifications (e.g. exercise and diet) and drugs that reduce heart rate, dilate blood vessels and/or increase urine production. Yet despite these numerous treatment options, more than 50 per cent of hypertensive patients fail to get their blood pressure under control.
Our team is investigating the role of the immune system, gut health and tissue fibrosis (scarring) in hypertension in the hope of discovering novel disease mechanisms and developing new drugs that are more effective at reducing blood pressure and protecting the heart, brain and kidneys from the damaging effects of hypertension.
Current Research Projects
We discovered that an immune complex called the NLRP3 inflammasome, contributes to the development of hypertension. Knocking out the genes that code for the NLRP3 inflammasome, or its cytokine product interleukin-18 (IL-18), reduces blood pressure, kidney injury and heart failure in mice with hypertension. Our current focus is on developing novel drugs that block IL-18 or its receptor and determining their effectiveness at treating hypertension and its downstream consequences of kidney disease and heart failure.
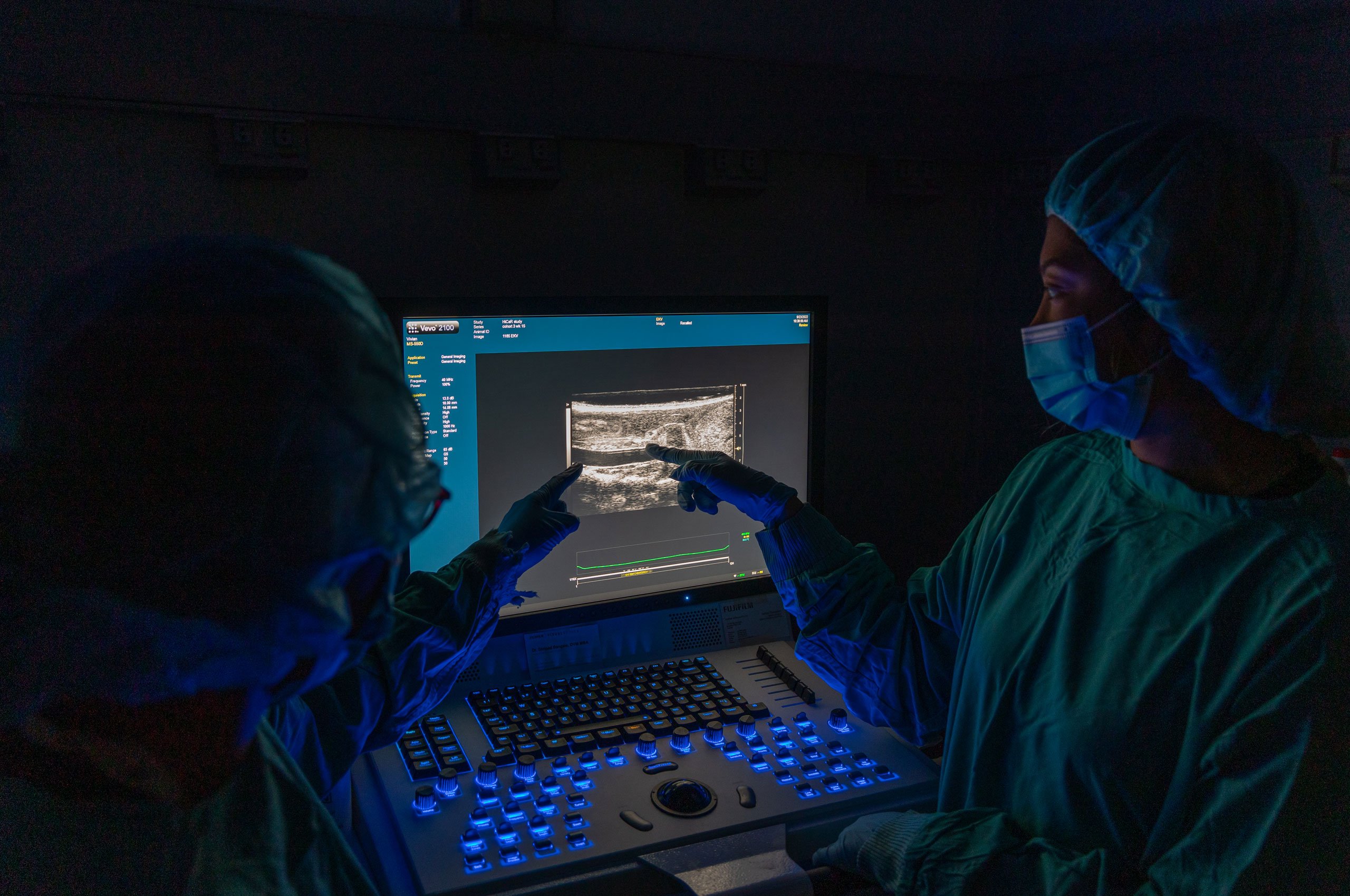
Classical autoimmune disorders occur when the body’s immune system turns on itself and mounts an attack against its own tissues, such as the joints in rheumatoid arthritis and the skin in psoriasis. The immune cells involved in these conditions are known as B and T cells. Our research has shown that B and T cells also play an important role in the development of hypertension by attacking key blood pressure-controlling organs such as the arteries, kidneys and brain. Using animal models of hypertension and powerful techniques such as confocal microscopy, flow cytometry and single cell RNA sequencing, we aim to define the stimuli that activate T and B cells during hypertension, as well as the factors these cells release to promote inflammation and damage in target organs. This knowledge will be used to devise new therapies to treat hypertension, including the possibility of repurposing drugs that are currently used to treat other autoimmune disorders.
As the largest artery of the body, the aorta plays a vital role in regulating blood flow to organs, as well as maintaining normal heart function. During hypertension, the aorta loses its elastic properties and becomes ‘stiff’, affecting its ability to perform these roles. To understand the causes of aortic stiffening, we have performed single cell RNA sequencing and spatial transcriptomic profiling of aortas isolated from mice with hypertension. New discoveries include identifying a novel cell population that is only present in diseased vessels. These novel cells appear to major producers of the rigid, structural protein collagen, making them prime suspects in the case to identify the cause of aortic stiffening. Our team is now exploring novel ways of inhibiting the function of these cells as a treatment for aortic stiffening.
Team members
Associate Professor Antony (Bill) Vinh (Division Head)
Dr Hericka Figueiredo Galvao (Postdoctoral Researcher)
Dr Vivian Tran (Postdoctoral Researcher)
Dr Courtney Judkins (Research Officer)
Tayla Gibson-Hughes (PhD Student)
Buddhila Wickramasinghe (PhD Student)
Jake Robertson (PhD Student)
Flavia Wassef (PhD Student)
Ghaida Moria (PhD Student)
Roberto Iaconis (Masters Student)
Vinh Nguyen Son Ngo (Honours Student)
