While this may sound strange, science does offer a plausible explanation.
Male pattern baldness is associated with high levels of male sex hormones called androgens. And androgens seem to play an important role in the entry of SARS-CoV-2, the coronavirus that causes COVID-19, into cells.
So it’s possible high levels of androgens might increase the risk of severe infection and death from COVID-19.
This hypothesis is important to identify people at risk and raises the possibility of new treatment strategies for COVID-19.
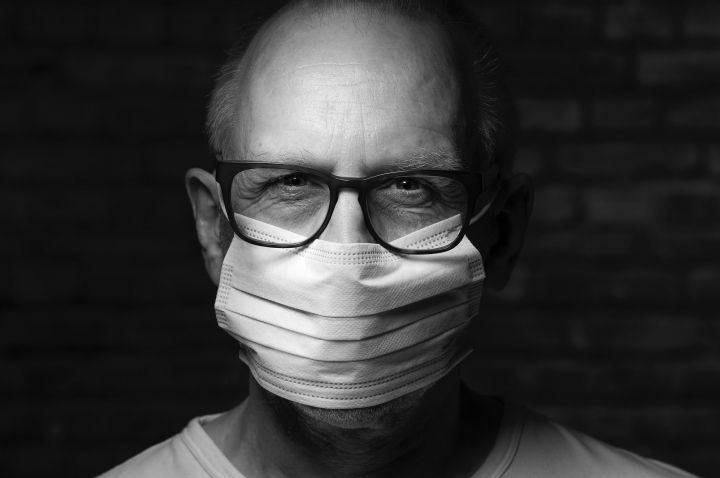
Men suffer more than women from COVID-19
It’s been obvious from early in the pandemic. Men are at greater risk of severe infection and death from COVID-19 than women.
There are several possible factors at play here. For one, men are more likely to suffer from chronic conditions known to pose a higher risk of serious illness from COVID-19. These include heart disease and diabetes.
Another is that men’s immune systems are not as good as women’s at warding off the severe effects of viral infections.
These factors are indirectly influenced by sex hormones. Now it seems sex hormones might also have a direct effect on SARS-CoV-2’s ability to enter our cells and establish infection.
Baldness and COVID-19
In one study of 122 male COVID-19 patients admitted to hospitals in Madrid, 79% were bald — about double the population frequency.
Another small study in Spain observed a similar overrepresentaton of baldness among men hospitalised with COVID-19.
Male pattern baldness is strongly associated with a higher level of dihydrotestosterone (DHT), a more active derivative of testosterone, and one of the androgen family of male sex hormones.
Confirming this correlation between baldness and susceptibility to COVID-19 with larger samples, controlling for age and other conditions, would be significant. It would suggest a higher DHT level could be a risk factor for severe COVID-19.
How does this link make biological sense?
SARS-CoV-2 enters human lung cells when a protein on the virus’ surface (the spike protein) latches onto protein receptors (ACE2 receptors) embedded in the cells’ surfaces.
How does this work? Recently scientists discovered that an enzyme called TMPRSS2 cleaves the SARS-CoV-2’s spike protein, enabling it to bind to the ACE2 receptor. This allows the virus to enter the cell.
The gene that encodes TMPRSS2 is activated when male hormones, particularly DHT, bind to the androgen receptor (a protein on the surface of cells, including hair cells and lung cells).
So the more male hormone, the more androgen receptor binding, the more TMPRSS2 is present, and the easier it is for virus to get in.
A preliminary, non-peer-reviewed study which correlated the androgen levels of hundreds of people in the UK with COVID-19 severity supports this theory. Higher androgen level was associated with susceptibility to and severity of COVID-19 in men (but not women, who have much lower androgen levels in their blood).
The same researchers showed that inhibiting androgen receptors reduced the ability of SARS-CoV-2’s spike protein to bind to ACE2 receptors on stem cells in culture.
Androgen disruptions are linked to different diseases
Over- or underproduction of androgens in the body causes a variety of conditions in both men and women.
For instance, men with benign prostate enlargement overproduce androgen, as do women with polycystic ovary syndrome.
Many such conditions are treated with androgen deprivation therapy (ADT), which inhibits the production or effect of androgens. For instance, prostate cancer, in which cancer cell growth is fuelled by androgens, is routinely treated with ADT.
Conversely, some people have low androgen production, or mutations that affect the binding and action of androgens — such as women with androgen insensitivity syndrome caused by mutations of the androgen receptor.
It will be important to find out whether, as the androgen hypothesis predicts, patients with over- or under-production of male hormones are at greater — or lesser — risk of COVID-19.
A potential treatment option?
If the androgen link holds up, this would encourage exploration of anti-androgens as a way to prevent and treat COVID-19.
Many anti-androgens are already approved for the treatment of other conditions. Some, like baldness treatments, have been used safely for years or decades. Some, like cancer treatments, can be tolerated for months.
A study which looked at men hospitalised with COVID-19 in Italy showed the rate of infection was four times lower in prostate cancer patients on ADT than in untreated cancer patients.
Perhaps a single dose given to someone who tests positive to SARS-CoV-2, or has just been exposed, would suffice to lower the chance of the virus taking hold.
But we need research to confirm this. Several androgen-suppressing drugs are now undergoing clinical trials to determine whether they reduce complications among men with COVID-19.
It will be important to verify that anti-androgen treatment works in the lungs as well as the prostate, and is effective in cancer-free patients. We’d also need to find out what dose is effective, and when it should be administered.
Anti-androgen treatments have several side effects in men, including breast enlargement and sexual dysfunction, so medical oversight is a must.
A promising new direction in COVID-19 research
The androgen link could go a long way to explaining why men are more susceptible to COVID-19 than women. It also may explain why children younger than ten seem very resistant to COVID-19 because, until puberty, boys as well as girls make little androgen.
The more we know about who is at heightened risk from COVID-19, the better we can target information.
The androgen link also opens up an avenue for the discovery of drugs which might mitigate some of the impact of COVID-19 as it continues to sweep the globe.
Originally published by The Conversation.